Technology-driven End-to-end Revenue Cycle
Management Services for Healthcare Providers
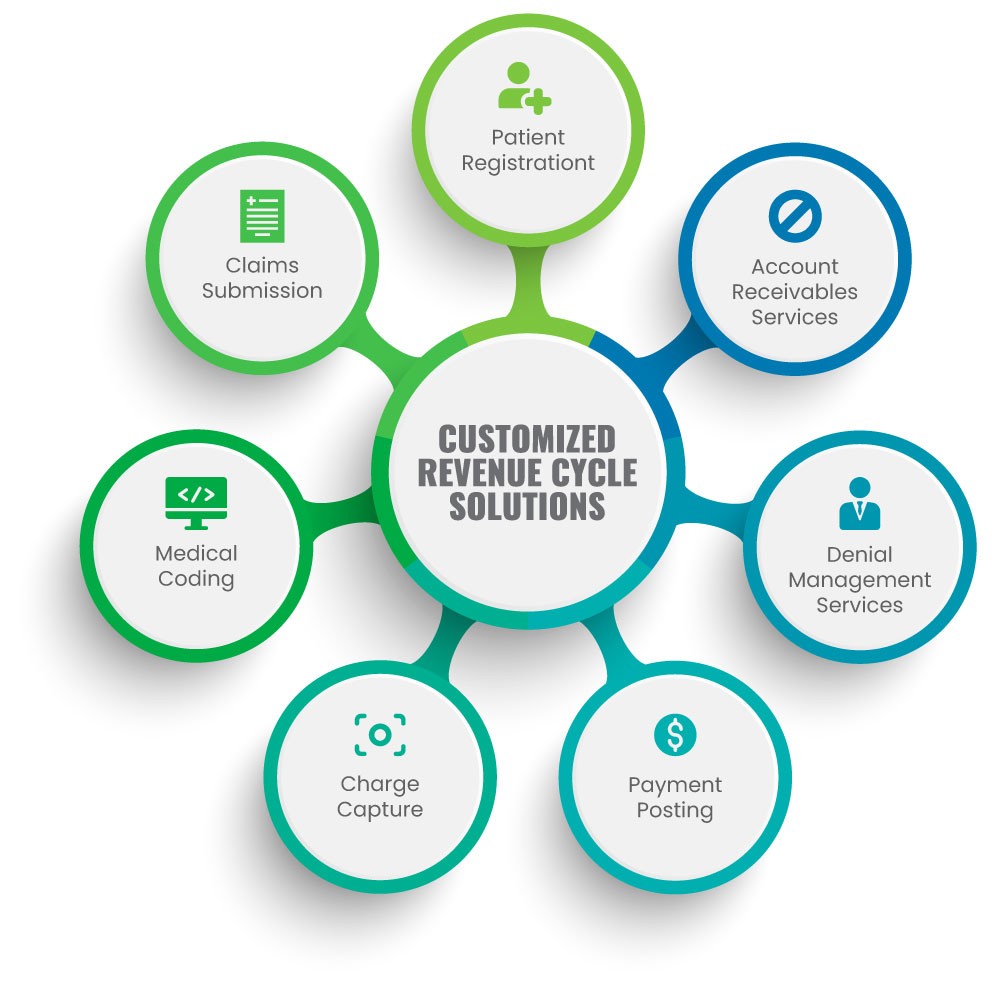
Managing accounts receivable efficiently while focusing on patient care is daunting for healthcare providers. At PreludeSys, we offer a holistic suite of medical billing, coding, and accounts receivable management services to guide you through the intricate web of administrative and clinical procedures.